ChatGPT Health and what AI can do for a broken system
Healthcare isn’t working for patients or doctors, but AI tools can help.
At this time last year, I was hospitalized for a kidney stone and developed an infection. The resident in charge took a quick look at my chart and prescribed the usual antibiotic for this kind of infection. Even though the nurse was ready to administer it, I asked her to give me a few minutes to get comfortable with the medication choice.
Because I’ve been dealing with a chronic illness for years, I had already uploaded a lot of my health records into ChatGPT. I asked whether I should be taking this antibiotic given my medical history, and ChatGPT flagged that this particular antibiotic could reactivate a very serious infection I’d had a couple of years prior.
When I brought this up with the resident, I expected pushback, but instead, she was relieved. She told me this medication could have created very serious complications for me, and she was glad I caught it. Naturally, I asked why this wasn’t caught by someone at the hospital instead, and she explained that she only has about 5 minutes per patient when making rounds, and that health records aren’t organized in a way that would make this sort of risk clear.
My experience exemplified why I believe so strongly in AI’s potential for health. 62% of Americans say our healthcare system is broken, and nearly half of U.S. physicians reported at least one symptom of burnout last year. The healthcare system clearly isn’t working for patients or doctors, which is why both are turning to AI tools for help, and why we built ChatGPT Health to support people even further.
According to the American Medical Association, physicians’ use of AI nearly doubled from 2023 to 2024, and 68% say AI gives them an advantage in being able to care for their patients. In a separate survey we commissioned, 3 in 5 US adults used AI tools for their health or healthcare over the past 3 months, and 75% of those who did found it very or extremely helpful.
When you look at what’s structurally wrong with healthcare today, it’s clear there’s a role for AI to play in addressing each one:
1. Doctors don’t have enough bandwidth.
Clinicians today have heavier caseloads and more administrative burden, which means less time with patients and even less time to keep up with the latest research. Under these conditions, it’s almost impossible for doctors to look beyond the immediate problem in front of them and see the full picture of someone’s health. That lack of context often means treating individual symptoms in isolation, rather than addressing the underlying drivers. This becomes an even greater challenge as more people live with multiple conditions at once, and many of these conditions sit at the intersection of genetics, environment, and lifestyle.
AI doesn’t have these constraints, which is why we see clinicians turning to AI tools to improve productivity on administrative tasks like note-taking, as well as support their clinical reasoning and serve as a second set of eyes to reduce diagnostic errors. AI systems are particularly good at synthesizing large amounts of information, which makes them well suited to helping doctors consider full medical histories, overlapping conditions, medications, and risk factors all together. AI can also help them draw on a growing body of medical research that no doctor can realistically track on their own when there are thousands of papers published every week.
In addition to supporting clinicians, AI can help make medical information more understandable for patients. Time constraints and language barriers mean doctors can’t always fully explain what they’re seeing and why they’re recommending a particular course of treatment. This is part of why 9 out of 10 U.S. adults say they can’t understand and use their own health information. But AI can translate that information into plain language and has infinite time for follow-up questions and explaining in a way that matches however you learn best.
2. The healthcare system is fragmented, while health requires looking at the full picture.
Having a chronic condition that affects multiple body systems has made it painfully clear to me just how fragmented our healthcare system is and how much of the burden falls to the patient to reconcile all of it. We have a world of specialists, each focused on a narrow piece of what’s going on with you, and who rarely work together. Unless you have the luxury of a concierge doctor, no one is looking at the full picture, which again is a problem when more and more of the diseases that afflict us don’t stay within a single organ or specialty. For my condition, I’ve had to see more than 20 specialists, each looking at a handful of symptoms out of dozens, even though my disease is systemic and affects nearly every part of my body.
This fragmentation extends to health data as well, with medical records spread across systems that don’t talk to each other. Only 16% of physicians fully exchanged and integrated electronic patient information as of 2021. The same goes for biosensor and wearable data, which most doctors don’t have the time or systems to review, unless it’s something narrow like blood glucose monitoring for diabetes. There have also been massive advances in genetics, but very few doctors systematically incorporate these signals into their daily practice.
With AI, we can finally break down silos and look at the full picture of a patient in a way that no part of the healthcare system is built to bring together today. I hear stories all the time about how this is empowering patients and their doctors to finally connect the dots that lead to diagnoses and treatments after years of dead-ends.
3. Cost and access are further barriers.
On top of all of this, cost and access keep many people from getting the care they need. Patients are navigating a complex system of referrals and insurance, and many end up with long wait times, rushed appointments, and often a big bill. These barriers are even greater in rural areas, where 10 hospitals per year have closed or shifted away from inpatient care on average since 2010. Many facilities that remain open are at risk of closure and have stopped offering important services like obstetrics or chemotherapy, which means people need to travel further, take more time off work, coordinate child care, and overcome other burdens that lead to delayed care and worse outcomes.
AI doesn’t replace expert medical care, but it can lower the friction to getting help, especially in moments when seeing a doctor isn’t feasible. Today we see 7 in 10 U.S. health conversations in ChatGPT happening outside of normal clinic hours. AI can also help with scheduling, researching providers, understanding insurance benefits, and other logistical tasks that take time and energy. For many families, these capabilities can be the difference between addressing a health concern early and waiting until something feels serious enough to justify the effort and expense.
4. Our healthcare model is reactive rather than preventative.
To improve your health, you can’t just do it when you’re sick; you need to work on it every day. According to the CDC, 5 of the top 10 causes of death in the U.S. are associated with preventable and treatable chronic diseases, but our system is set up around going to see a doctor only when something is wrong. Things like nutrition, physical activity, sleep, and stress all play an outsized role in health, but most people are left to manage them on their own. Even when clinicians know that behavioral changes matter more than another prescription, they don’t have a way to truly support patients outside the clinic. Structured meal plans, healthy groceries, gym memberships, trainers, or other wellness programs are rarely covered by insurance, and they require time and money that many people simply don’t have. This creates a cycle where instead of addressing the root issue, we wait until things get bad enough to go back to the doctor.
Now with AI, anyone can have a daily companion to support their health journey. Instead of trying to interpret nutrition advice on their own, people are asking ChatGPT to look at a restaurant menu or a product’s nutrition facts to figure out what fits their dietary needs. When they hit a wall at the gym, they turn to ChatGPT for ideas and motivation to stay active. By helping people make better choices in the moment and stick with healthy habits, AI can make managing your health an ongoing practice that feels achievable instead of overwhelming.
Why we built ChatGPT Health
With more than 40 million people globally turning to ChatGPT every day for health questions, we’re starting to see how AI can help address the shortcomings of the current healthcare system. To make an even greater impact, we need to make it much easier for anyone to discover what’s possible with ChatGPT and get the full value out of it for their health. For example, it’s a pain to go through several different health systems, figure out how to download your files, and then upload them all into ChatGPT.
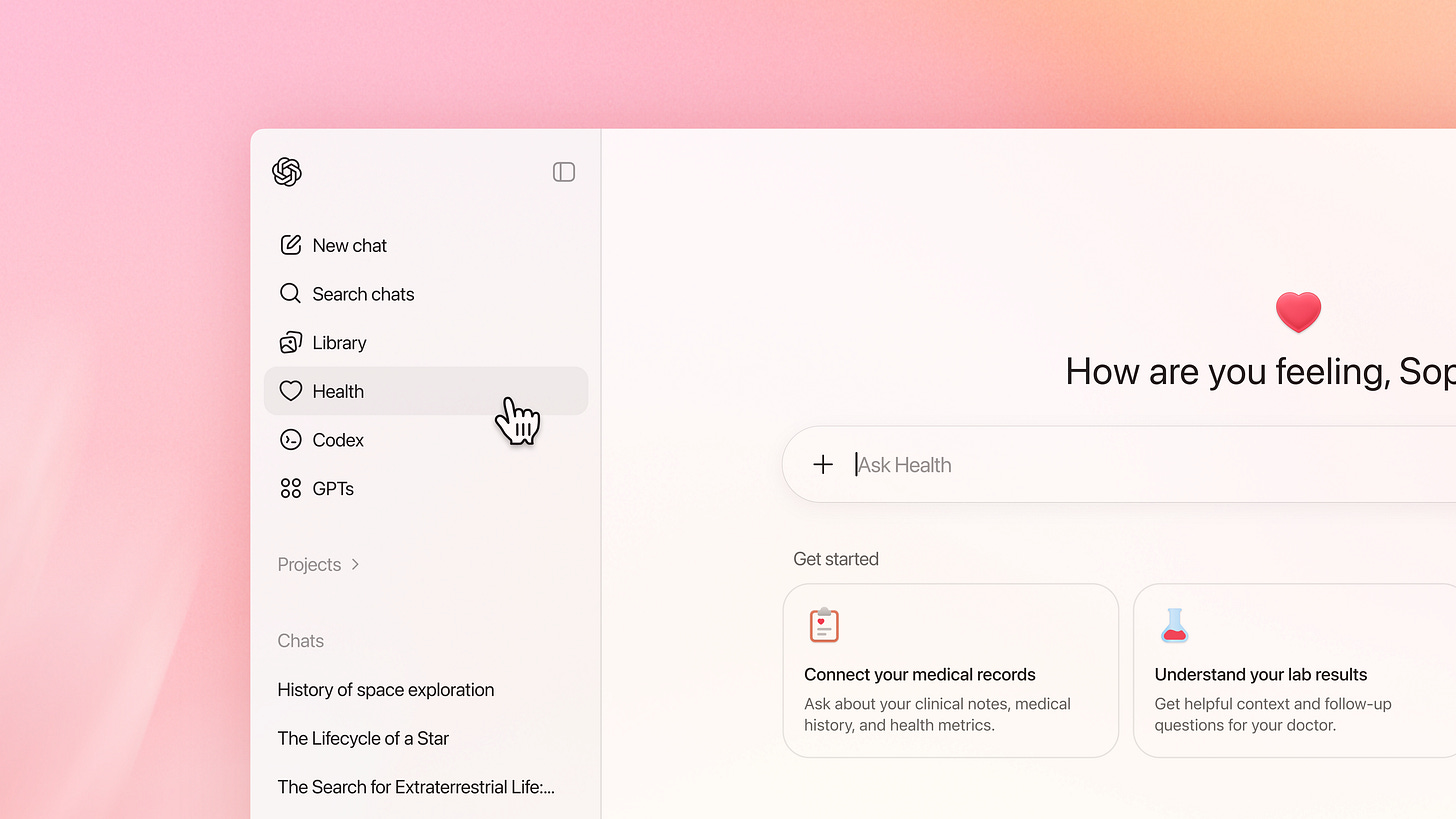
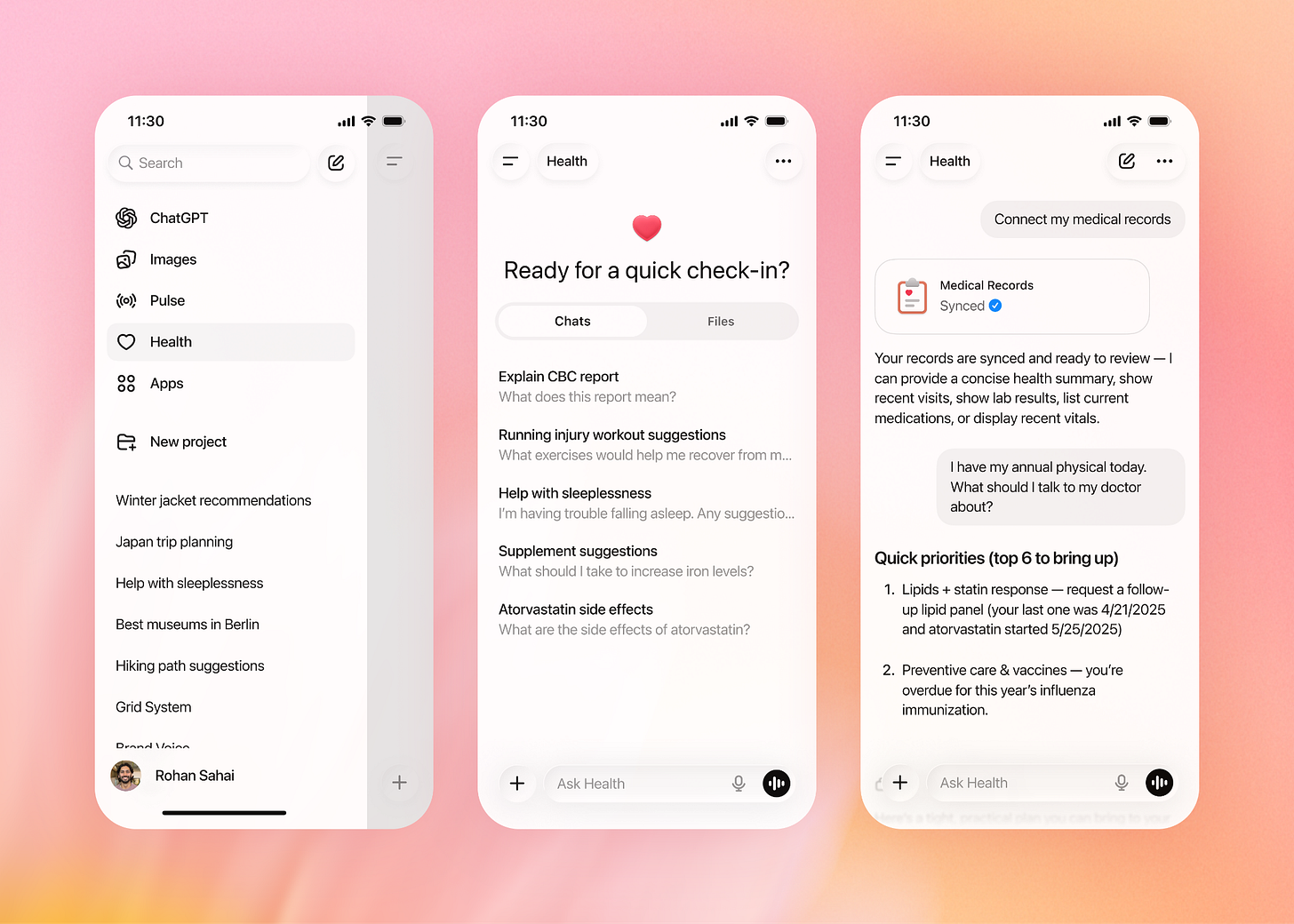
That’s why today we’re launching ChatGPT Health, a dedicated, private space for health conversations where you can easily and securely connect your medical records and wellness apps, like Apple Health, Function Health and Peloton. This allows ChatGPT to offer more relevant, personalized support, like when you’re preparing for a doctor’s appointment or looking for guidance on a meal plan or exercise routine that fits your needs.
ChatGPT Health is another step toward turning ChatGPT into a personal super-assistant that can support you with information and tools to achieve your goals across any part of your life. We’re still at the very beginning of this journey, but I’m excited to get these tools into more people’s hands. You can sign up to request access to ChatGPT Health here. You can also read our blog post for more information about how ChatGPT Health works and how we developed it with strong privacy protections and input from physicians.

Curious if you can go into more detail on the differences in training/tuning between the Health model and the public release model. We all know the Public model is flawed and hallucinates more than it doesn't, very curious how someone could trust their Health to the tool. Also, did you not just come out a month or so back and say that ChatGPT should not be used for Medical Advice?
Great start and all very valid reasons for ChatGPT to focus on health. I have two big questions:
1. Will all of my conversations with ChatGPT Health be hippa compliant (meaning my personal information will not be used in any way other than patient/provider communication?)
2. When with this connect to my medical records housed within Epic or Oracle (Cerner) so that I can start to have that "holistic" picture that you describe?